Joint contracture - description, treatment. Contractures of different groups of joints, causes, symptoms and methods of treatment Flexion contracture mkb 10
Excluded: free body in knee joint(M23.4)
Excluded:
- chondrocalcinosis (M11.1-M11.2)
- intra-articular lesion of the knee (M23.-)
- disorders of calcium metabolism (E83.5)
- ochronosis (E70.2)
Instability due to old ligament injury
Weakness of ligaments NOS
Excludes: displacement or dislocation of joint:
- congenital - see congenital malformations and deformities of the musculoskeletal system (Q65-Q79)
- current - see injuries of the joints and ligaments by area of the body
- repetitive (M24.4)
Excluded:
- acquired limb deformities (M20-M21)
- sheath tendon contracture without joint contracture (M67.1)
- Dupuytren's contracture (M72.0)
Excluded:
- spine (M43.2)
- joint stiffness without ankylosis (M25.6)
Excludes: iliac tibial ligament syndrome (M76.3)
In Russia, the International Classification of Diseases of the 10th revision (ICD-10) is adopted as a single regulatory document for accounting for morbidity, reasons for the population to apply to medical institutions of all departments, and causes of death.
ICD-10 was introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997. №170
The publication of a new revision (ICD-11) is planned by WHO in 2017 2018.
With amendments and additions by WHO.
Processing and translation of changes © mkb-10.com
Dupuytren's contracture
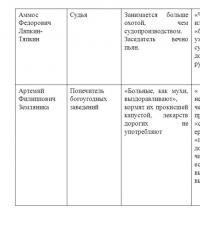
type of middle age - differs in a less intense course than the senile type, somewhat limits the ability to work;
female type - occurs in women, while significant progression is not observed;
explosive type of flow - characterized by high activity of fibroplastic processes, significant functional disorders and a tendency to relapse.
- Stage 1 - the presence of nodes or strands in the palm area in the absence of contractures and functional disorders;
2nd stage - the beginning contracture of one or more metacarpophalangeal joints;
Stage 3 - significant contractures of the metacarpophalangeal joints and incipient contractures of the proximal interphalangeal joints;
Stage 4 - pronounced contractures of the metacarpophalangeal and proximal interphalangeal joints with hyperextension of the distal interphalangeal joints.
With KD, 3 stages of the disease are traditionally distinguished:
- 1st stage - the appearance of changes in the palmar aponeurosis (nodules, very stable and immobile, strands) without contracture of the fingers;
Stage 2 - the appearance of contracture of the fingers (limitation of extension in the metacarpophalangeal joints) and skin lesions;
Stage 3 - a pronounced contracture of the fingers in the flexion position (extension is impossible) with the development of secondary changes in the skin and interphalangeal joints of the fingers.
Distinguish isolated contracture of one, more often IV or V, finger and widespread KD - on all fingers. A typical form of CD - the development of contracture begins with the palm, with an atypical form - from the finger. According to the prevalence, palmar, finger and palmar-finger forms are distinguished:
- digital form - characterized by the development of pathological changes, as a rule, in the longitudinal cords of the aponeurosis within the finger; at the same time, flexion contracture of the proximal interphalangeal joints (PMFS) and extensor contracture in the distal interphalangeal joints (DMFS) occur; occurs in 10% of cases;
palmar form - characterized by damage to the longitudinal bundles of the aponeurosis within the palm; there are no pathological changes on the fingers, and only the metacarpophalangeal joints (PFJ) are in a state of flexion contracture; observed in 30% of cases;
mixed palmar-natal form - longitudinal bundles on the hand and fingers are affected; PFJ, PMFS, and sometimes DMFS are in a state of flexion contracture; this form occurs most often - in 60% of cases.
The data of specialized literature show that in clinical practice, the classification of KD according to the degree of deformity and dysfunction of the hand is most often used. It meets modern requirements and corresponds to four degrees of functional disorders. In accordance with this classification, 4 degrees of flexion contracture of the fingers are distinguished:
- I - from 0° to 35°;
II - from 35° to 70°;
III - from 70° to 90°;
IV – from 90 to 135°.
This classification meets modern requirements and corresponds to the 4th degree of functional disorders given in the regulatory documents of medical and social expertise - ITU (see Order of the Ministry of Health and Social Development of Russia dated August 22, 2005 No. 535 “On approval of classifications and criteria used in the implementation of medical and social expertise federal citizens government agencies medical and social expertise"). In accordance with this classification, 4 degrees of flexion contracture of the fingers are distinguished:
- I degree (minor dysfunction of the hand) - subcutaneous nodes in the palmar aponeurosis: patients complain of a feeling of "swelling" of the hand in the morning, "fatigue" in the hands, "numbness" of the fingers, cold fingers even in warm weather; typical subcutaneous nodular seals are formed on the palmar surface of the hand, subsequently turning into a dense knot or cord that captures the skin and subcutaneous tissue and goes to the base of one or another finger; the function of the fingers and hand is not impaired;
II degree (moderate dysfunction of the hand) - persistent flexion contracture of one finger (usually IV or V) in the metacarpophalangeal and proximal interphalangeal joints, not exceeding an angle of 90 °; flexion of the fingers is preserved, the function of the hand is moderately impaired;
III degree (pronounced dysfunction of the hand) - flexion contracture of the fingers at an angle of 90 °, the fingers are maximally bent, the fingertips touch the palm, the movements of the fingers are impaired; as a result of wrinkling of the articular bags, subluxations of the phalanges of the fingers are possible; pronounced dysfunction of the hand without pain;
IV degree (significantly pronounced dysfunction of the hand) - flexion contracture of the fingers at an angle of at least 90 °, pronounced, there are arthrogenic contractures, dislocations of the phalanges; significantly pronounced dysfunction of the hand; pain is usually absent; in some cases, another hand and feet can be simultaneously affected (Ledderhose's disease - contractures of the plantar aponeurosis of the feet), more rarely - the cavernous bodies of the penis (Peyronie's disease).
Diagnostics. The diagnosis is made on the basis of clinical examination, palpation, assessment of the prevalence of the process and functional disorders of the main functions of the hand (grasping and holding objects) and includes, according to indications, radiography of the hand, rheovasography, EEG and other special methods. Differential diagnosis is carried out with visually similar diseases: neurogenic, traumatic, rheumatoid and ischemic contractures, scleroderma, hygromas and fibromas of the synovial-aponeurotic canals, tendovaginitis, stenosing ligamentitis and some congenital anomalies (campto- and clinodactyly).
Dupuytren's contracture - description, causes, symptoms (signs), treatment.
Short description
Dupuytren's contracture is a painless thickening and shortening of the palmar fascia due to fibrous tissue proliferation, leading to flexion deformity and loss of hand function. The predominant age is over 40 years. The predominant gender is male (10:1).
Causes
Risk factors Chronic trauma Brachial plexus neuropathy Rare hereditary syndromes
Pathomorphology Fibrosis and signs of inflammation are found in the palmar fascia and adjacent flexor tendon sheaths. The same changes are sometimes found in the plantar fascia.
Symptoms (signs)
Clinical picture Changes can be both unilateral and bilateral. With a unilateral process, the right hand is more often affected. The ring finger is most often deformed, then the little finger, middle and index fingers. At the beginning of the disease, small, painless, dense nodules appear in the palmar fascia, which then combine into a longitudinal band. The cord is soldered to the skin and surrounding tissues. The skin becomes folded, flexion contractures gradually develop. The fingers are bent at the metacarpophalangeal joints to an angle of 100°, active and passive extension of the fingers is impossible. The nodules are palpated under the skin folds or over the joints. In the later stages of the disease, the fingers are bent at the metacarpophalangeal joints to an angle of 90 °, in the proximal - from a blunt to a right angle (often the nail phalanx is pressed against the palm), extension of the fingers is impossible.
Concomitant pathology Ledderose's disease - damage to the plantar fascia Peyronie's disease (171000, Â) - damage to the fascia of the penis.
Treatment
Treatment Conservative treatment is ineffective: prescribe injections into the tissues of the altered tendon sheaths of hydrocortisone, lidase, phonophoresis with hydrocortisone, mud applications, dressings with dimethyl sulfoxide, injections of the vitreous body, aloe; massage, therapeutic exercises, physiotherapy Surgical treatment - the technique depends on the stage of the disease: subcutaneous fasciotomy, limited fasciectomy, radical fasciectomy.
Synonyms of Dupuytren's syndrome Contracture of the palmar aponeurosis
ICD-10 M72.0 Palmar fascial fibromatosis [Dupuytren].
Palmar fascial fibromatosis [Dupuytren]
Definition and background[edit]
Palmar fascial fibromatosis (Dupuytren's contracture) is characterized by fibrosis of the palmar fascia and fascia of the fingers.
Dupuytren's contracture most often affects the ring finger, less often the little finger and middle finger (thumb and forefinger are usually not involved).
Etiology and pathogenesis[edit]
Dupuytren's contracture is an apparently genetic epidermal disease.
Clinical manifestations[edit]
The earliest clinical manifestations are painless strands or nodules in the thickness of the skin or under it in the area of the palm closer to the metacarpophalangeal joints, limitation of passive extension of the fingers, discomfort, pain, feeling of tightness, contraction of the palm when moving the fingers, morning stiffness.
Palmar fascial fibromatosis [Dupuytren's]: Diagnosis[edit]
Differential diagnosis[edit]
Palmar fascial fibromatosis [Dupuytren's]: Treatment[edit]
The goal of treatment is to eliminate inflammation in the tissues, focal contracture of muscle fibers, restore the function of the affected muscles, ligaments and tendons.
Physical therapy of patients with soft tissue diseases is aimed at combating pain (analgesic methods), inflammation (anti-inflammatory methods) and increasing the functional properties of affected tissues (fibromodulating methods).
Dupuytren's contracture
ICD-10 code
Titles
Description
This disease varies in its degree of progression, from slight wrinkling of the skin, which can last for many years, to the rapid formation of contracture (fixed position).
Symptoms
With the progression of this disease, it becomes impossible to straighten the fingers. As a result, the ability to pick up objects may be lost.
This disease is rarely accompanied by pain, unless the affected fingers are inadvertently or deliberately stretched out.
Causes
This disease can be transmitted genetically, in an autosomal dominant pattern with incomplete penetrance and partial sex restriction. This means that the gene responsible for the development of this disease is located neither on the X nor on the Y chromosome (sex chromosomes), but on one of the 44 chromosomes. Therefore, one version of this gene will be quite enough for the development of this disease (it dominates), but not all people who have this species gene inherit the disease (this gene is not completely penetrant), and therefore the disease is most often seen in males (gene expression is partly restricted to the male sex).
Treatment
Many patients with this disease require support and warm compress stretching exercises. If the palm is very sensitive to grasping, ultrasound treatment may help. Sometimes corticosteroid injections are the best treatment for local inflammation.
Surgery may be needed for those patients who have extensive disease to remove the scar tissue and free the fingers. With the help of such operations, you can restore the hand to its former mobility. Small nodules and / or thickening of the skin on the palm of your hand is not a reason for surgery. Sometimes the surgeon can gently remove the scar tissue with a needle. This procedure is called needle aponeurotomy.
Diseases: Palmar fascial fibromatosis [Dupuytren]. Code according to mkb-10
Nizhny Novgorod, 2013
Loos B., Puschkin V., Horch R.E., 2007.
Bainbridge C. et al., 2012.
Bainbridge C. et al., 2012.
Loos B., Puschkin V., Horch R.E., 2007.
Loos B., Puschkin V., Horch R.E., 2007.
Loos B., Puschkin V., Horch R.E., 2007.
Skin flap necrosis
Marginal necrosis of the skin flap
Fedutinov D.A. et al., 2008.
Fedutinov D.A. et al., 2008.
Bainbridge C. et al., 2012.
Persistent pain syndrome
Bainbridge C. et al., 2012.
The number of relapses of the disease after surgical treatment ranges from 7 to 27% (Abe Y. et al., 2004; Anwar M. U., Al Ghazal S. K., Boome R. S.,2007; H ö Gemann A. et al., 2009). The risk of contracture recurrence does not decrease even five or more years after the operation (Meinel A., 1999).
Insufficient knowledge of the anatomy of the hand. Damage to nerves and arteries occurs when these structures are displaced by scars, and the surgeon, following the standards of anatomy, excised scars where, in his opinion, nerves and blood vessels should not be;
Non-rational accesses that do not take into account the sources of blood supply to the skin of the hand and the location of scar-changed aponeurosis cords;
Significant tissue trauma during the operation due to lack of instruments, equipment and insufficient experience;
Neglect of careful hemostasis, which leads to the formation of extensive hematomas in the beds of the hand, slowing down the healing process of wounds, leading to the formation of massive scars;
Excision of only a roughly altered part of the aponeurosis or its dissection, which very quickly leads to a relapse;
Underestimation of the importance of therapeutic measures in the postoperative period.
One cannot but agree with A.V. Zhigalo (2010) that there is still no single rational surgical approach for the treatment of patients in this category. At the same time, even among experienced hand surgeons there are no common views on the scope of the operation, surgical technique, surgical approaches, as well as tactics. postoperative treatment and rehabilitation of patients.
Dupuytren's contracture and its treatment
Dupuytren's contracture is a fibrous degeneration of the palmar aponeurosis that results in flexion contracture of the fingers. The second name of the disease is palmar fibromotosis. The disease is more common in men over the age of 40. The pathological process has a slow progressive course, causes a violation of the motor activity of the hand and forms a disability in case of damage to the working upper limb. In most clinical cases, the 4th and 5th fingers (ring and little fingers) on one hand are affected. Less commonly, all fingers on both hands or feet are involved in the pathological process. In the international classification of diseases or ICD 10, pathology is assigned code M 72.0.
Causes of the disease
Dupuytren's contracture develops as a result of sclerotic processes in the tissue of the palmar fascia. Under the skin of the palm is the palmar aponeurosis, which protects the tendons of the hand, blood vessels and nerves from damage and is involved in the flexion-extensor movements of the fingers. In rare cases, the pathological process develops in the plantar fascia of the foot, which performs similar functions.
In palmar fibromatosis, the ring finger and little finger are usually affected.
Due to the influence of adverse factors, fibrous nodules and strands are formed in the fascia, causing wrinkling and deformation of the aponeurosis. As a result, there is a pathologically forced position of the fingers in a state of flexion at a different angle to the palm. Extension of the fingers becomes difficult or impossible, which eventually leads to ankylosis (immobility) of the interphalangeal and metacarpophalangeal joints. In this case, the brush loses its functional activity. This causes loss of ability to work and self-care skills.
Modern medicine considers hereditary predisposition to be the main cause of the disease. The pathology is associated with a defective gene, which increases the risk of contracture in members of the same family and close relatives.
For the manifestation of a genetic mutation, the impact of adverse factors is necessary:
- hand or foot injury;
- heavy physical labor;
- endocrine pathology (thyrotoxicosis, diabetes mellitus);
- chronic liver diseases;
- alcohol abuse;
- nicotine addiction;
- epilepsy.
The disease is named after the French surgeon Guillaume Dupuytren, who at the beginning of the 19th century proposed a radical method of treating contractures - the aponeurotomy operation.
Clinical picture
Dupuytren's contracture is more common in men over the age of 40. In this case, the disease has a slow progressive course. If the disease develops at a young age, it is usually characterized by an acute onset and a rapid increase in sclerotic changes in the palmar aponeurosis. Clinical manifestations of contracture are in violation of the work of the hand due to forced flexion of the fingers. Anatomical and functional disorders occur several years or a decade after the onset of the first symptoms of pathology.
Clinical manifestations of contracture progress slowly
The initial manifestations of the disease are accompanied by the formation of painless seals on the palmar surface of the hand, which are formed during focal sclerosis of the fascia. The progression of the pathological process leads to an increase in areas of fibrosis with spread to the area of the fingers. Wrinkling of the palmar aponeurosis causes a change in the skin of the palm and gives the skin the appearance of parchment paper.
Shortened fascia contributes to the appearance of flexion contracture and makes it difficult to independently extend the fingers.
Prolonged position of the hand in an unnatural position forms ankylosis of the joints. The progression of the pathology leads to the appearance of pain in the area of fibrous cords, which makes patients seek medical help.
Compression of the nerves and blood vessels by strands causes trophic skin disorders (dryness, peeling, chilliness of the hands) and a decrease in the sensitivity of the fingers. With the defeat of the ring finger and little finger, the hand takes the form of an "obstetrician's hand". This form of the hand leads to a permanent dysfunction of the upper limb and causes a decrease in working capacity.
Fibrosis of the soft tissues of the palm and fingers in Dupuytren's contracture
According to the nature of the violation of the motor function of the fingers, 4 degrees of Dupuytren's contracture are distinguished.
- The first degree - is not accompanied by a violation of the extension of the fingers.
- The second degree - the deficit of extension of the fingers does not exceed 30 degrees.
- The third degree - the deficit of extension of the fingers is in the range from 30 to 90 degrees.
- Fourth degree - the deficit of extension of the fingers is more than 90 degrees.
To increase the effectiveness of therapy, it is necessary to consult a doctor in the first stages of the disease. Advanced cases of the disease lead to damage to the vessels and nerves of the hand, complete immobility of the fingers, which necessitates amputation of the affected anatomical structures.
Diagnosis and treatment
When clinical signs of the disease occur, the doctor usually does not have difficulty in making a diagnosis. When first seeking medical help from a traumatologist or surgeon, the doctor finds out the patient's complaints, the causes of the disease, evaluates the mobility of the fingers. To confirm the diagnosis, x-rays and ultrasound of the hand are prescribed, which helps to identify the degree of damage to the joints and palmar fascia.
Treatment of Dupuytren's contracture is carried out conservatively and surgically. Without surgery, the initial forms of the disease are treated, which are not accompanied by significant flexion contracture of the fingers. Conservative therapy is aimed at preventing the progression of the pathology, eliminating the pain syndrome, and improving the motor activity of the hand.
Soft tissue incision line during surgery
Conservative treatments for Dupuytren's contracture:
- introduction by injection into the palmar aponeurosis of the collagenase enzyme to remove fibrous bands;
- skin application or electrophoresis of a collalizin solution to prevent cicatricial changes in the skin of the palms and feet;
- longet bandages on the brush for extension of the fingers (applied at night);
- novocaine blockades with the addition of glucocorticoids (diprospan, kenalog) to reduce pain in the arm;
- warm baths for hands and feet;
- massage of the hands and feet;
- physiotherapy (electrophoresis with novocaine, UHF, paraffin applications);
- therapeutic exercises to develop joints and increase the elasticity of the palmar fascia.
Conservative therapy only stops the development of the disease. The effectiveness of treatment increases the rejection of addictions. To radically get rid of contracture, an operation is performed, the volume of which depends on the severity of anatomical and functional disorders. The operation is usually prescribed for 3-4 degrees of the disease. During surgery, partial or complete removal of the palmar aponeurosis is performed.
Types of operations for Dupuytren's contracture:
- partial excision of the palmar aponeurosis in the area of localization of fibrous cords;
- complete removal of the palmar fascia with significant flexion contracture of the fingers;
- arthrodesis in the advanced stage of the disease, which is accompanied by impaired mobility of the metacarpophalangeal and phalangeal joints;
- amputation of fingers when joints, nerves, blood vessels are involved in the pathological process.
Rehabilitation after surgery consists in the appointment of conservative methods of therapy: physiotherapy, massage, physiotherapy exercises (exercise therapy).
Reviews of patients about the treatment of the disease
Currently, there is no consensus among physicians about the timing of the appointment of conservative methods and surgical intervention. In the case of the onset of the disease in adulthood, after years the pathology has a slow progressive course and responds well to conservative treatment. The appearance of pathology at a young age increases the risk of rapid formation of flexion contracture and ankylosis of the finger joints, which indicates in favor of the operation.
In some cases, the pathological process behaves unpredictably, which requires constant monitoring of the patient by a specialist. The doctor chooses the method of therapy in each case, based on the age of the patient, comorbidities, professional activity. Below are the reviews of patients about various types treatment of the disease.
Joint changes during contracture formation
Maxim Alexandrovich, 30 years old. I work as a mechanic in a factory. A year ago, a small seal appeared on the right palm, which did not cause discomfort. A few months later, the seal increased in size and such “bumps” formed on the left arm. There were pains in the hands, growing towards the end of the working day. Over time, I began to notice the constant flexion of the ring finger, which was difficult to unbend. The inability to work with his hands forced him to turn to a surgeon. An operation was performed for palmar fibromatosis, after which he returned to work. Fingers work normally, pains have stopped.
Sergey Nikolaevich, 48 years old. In my family, my father and older brother were diagnosed with Dupuytren's contracture. Therefore, after the appearance of a small “bump” on the right palm, he immediately went to the doctor. Periodically I do injections with collagenase, undergo physiotherapy, massage the hands and develop my fingers with the help of special exercises. For 10 years, several new seals have appeared on the palms of the hands, but the movements of the fingers are free. The doctor said that with constant monitoring and treatment, the operation would not be required.
Anna Ivanovna, 53 years old. She underwent surgery for palmar fibromatosis of the right hand 10 years ago. Five years later, the disease appeared on the left arm. Every year I go through massage courses, develop brushes with the help of therapeutic exercises, and do electrophoresis with collalizin. Despite the treatment, it is difficult to unbend the fingers of the hand, pains appeared in the arm. I'm getting ready for another operation.
Dupuytren's contracture is a progressive disease of the palmar aponeurosis that leads to finger flexion and dysfunction of the hand. A timely visit to the doctor helps to improve the prognosis of the pathology and allows you to maintain the work of the hand with conservative methods. Late stages of the disease are subject to surgical treatment and may lead to amputation of the fingers.
Contracture of the fingers treatment
Symptoms and diagnosis of Dupuytren's disease - treatment, surgery and rehabilitation course
Dupuytren's palmar fascial fibromatosis is a non-inflammatory disease that causes scarring of the palmar tendons. This disease affects the inhabitants of Scandinavia, Ireland and Eastern Europe. Dupuytren's contracture is characterized by the fact that in a patient one or two fingers cease to unbend, a kind of bump forms in the area of the affected tendons, and the hand partially loses its functions.
What is Dupuytren's contracture
The disease resulting in a deformity of the hand is Dupuytren's contracture. The disease affects the ring finger and little finger. Dupuytren's syndrome develops with excessive development of connective tissue, leading to a reduction in the fascia in the palm of your hand. The ICD-10 code is M72.0. The disease is not associated with disorders of carbohydrate, protein or salt metabolism. As a result of the pathological process, the patient loses the ability to unbend one or two fingers, in advanced cases stiffness of the fingers develops. The disease can degenerate into a lesion of the aponeurosis of the feet.
At the moment, the exact causes of contracture of the fingers have not been established. The onset of the disease is influenced by heredity, age (it is very rare in young people). In men, contracture occurs more often, develops more rapidly compared to women. Smoking and alcohol abuse increase the likelihood of Morbus Dupuytren disease. Another factor that increases the risk of the disease is diabetes mellitus.
Doctors distinguish the following signs of the disease:
- Impaired ability to extend fingers.
- Stiffness of the joints of the involved fingers.
- development of ankylosis.
- Deformities of the hand, the occurrence of compaction in the palm of your hand.
- Formation of subcutaneous indurations that thicken over time.
The contracture of the fingers develops without certain patterns. In some cases, for many years, Dupuytren's disease remains at the initial stages, in others - in a few months the disease reaches the last stage. Depending on the severity of symptoms, there are three degrees of palmar aponeurosis:
- First. The diameter of the nodular outgrowth on the palm does not exceed 1 cm. The cord may appear on the palm or in the area of the metacarpophalangeal joint. It is possible to treat Dupuytren's contracture without surgery.
- Second. The cord is located in the region of the main phalanx, becomes more dense and coarse. The skin on the palm of the hand roughens, funnel-shaped depressions and retracted folds form at the site of the lesion. The affected fingers are bent at the metacarpophalangeal joint at an angle of 100 degrees, completely losing the ability to unbend.
- Third. The cord is formed on the middle or nail phalanges. Flexion and extension movements are limited. The phalanges are located to each other at an angle of 90 degrees, ankylosis is possible.
Diagnosis of Dupuytren's contracture
The diagnosis begins with a questioning of the patient: the doctor needs to know about the patient's complaints, the impact of contracture on the quality of life, and the duration of the course of the disease. The doctor may ask if the patient is abusing alcoholic drinks and smoking, about cases of contracture of the patient's relatives. The next stage of diagnosis is a physical examination. The doctor examines and palpates the hand, examines the amplitude of flexion and extension of the fingers. Laboratory and instrumental methods are not used to diagnose the disease.
Treatment of Dupuytren's contracture
The branches of medicine are engaged in the treatment of the disease: orthopedics, surgery, traumatology. Operative and conservative methods of therapy are used. For pain syndrome, therapeutic blockades with hormonal drugs (Diprospan, Triamcinolone, Hydrocortisone) are used. Treatment of neurogenic contracture without surgery is possible only in the initial stages. If you do not see a doctor in time, you may need to amputate your finger.
Operational
Treatment of contracture of the fingers occurs with the help of surgical intervention methods:
- Aponeurectomy. Shown when the finger is flexed 30 degrees or more. With a partial aponeurectomy, only the aponeurosis with scarred tissue is removed. The operation takes a long time, but not always the palmar aponeurosis, not always altered by scars, is completely removed.
- Aponeurotomy:
- Needle fasciotomy. With the help of a needle, the doctor dissects cicatricial changes in the palm and fingers. Gradually, the ability to straighten the fingers is fully restored. This method has practically no contraindications, guarantees low trauma, and when all instructions are followed, it provides quick rehabilitation, the resumption of the extensor function immediately after the operation.
- Open fasciotomy. Carried out in the last stages of the disease under local anesthesia. The doctor makes an incision at the site of scarring and cuts the damaged tissue. After a reconstructive operation, the aponeurosis may heal again, which will lead to a second visit to the doctor. The risks of the operation are much higher compared to needle fasciotomy, and reviews are conflicting.
Collalysin
How to treat Dupuytren's contracture if surgery is contraindicated? In such cases, injections of collalizin are recommended. The patient is injected with Xiaflex into the healed fascia. The medication provokes its decay and the disappearance of the scar. The procedure is performed on an outpatient basis and takes about half an hour. After the end, the patient is put on a bandage or splint. The scar dissolves the next day, leaving no marks on the skin. After the injection, the ability to straighten the fingers is fully restored.
Folk remedies
Treatment folk remedies can be used as an addition to traditional methods. For treatment at home, folk methods are used:
- Baths. Thermal procedures improve blood circulation. Hands are steamed in a saline broth of chamomile, sage, vegetable peel.
- Compresses. For a compress, black poplar buds, mordovnik seeds, horseradish root, vodka are used.
- Rubbing. The brushes are rubbed with tinctures from vegetable oils with the addition of red pepper, rubbing from the infusion of chestnuts gives a good effect.
Physiotherapy
The goal of therapeutic exercises is to improve the elasticity of the aponeurosis and increase the motor activity of the finger joints. Every two hours, you need to unbend and bend your fingers about 20 times. Before and at the end of the exercise, massage the hands, and for the best effect, it is recommended to use a rubber expander. Every day you need to increase the number of repetitions, pain in muscles and ligaments is allowed.
Video: palmar fibromatosis
Dupuytren's contracture and Volkmann's contracture - treatment of diseases
Contracture is a condition in which the range of motion in a joint is limited or completely absent. By origin, contracture is divided into acquired and congenital. Congenital include torticollis, clubfoot, etc. Acquired belongs to Dupuytren's syndrome, Volkmann's ischemic contracture, dermatogenic contracture, etc.
What is Volkmann's contracture
Volkmann's contracture ("clawed foot", "claw-like hand", ischemic paralysis) - restriction of hand mobility due to prolonged disruption of arterial blood supply to the muscles of the hand.
A fracture of the forearm, trauma to the bones, muscles and ligaments of the arm can lead to impaired blood flow.
The most frequent cases of Volkmann's ischemic contracture are seen with a fracture of the shoulder with damage to the brachial artery. To limit the flow of blood to the hand, a small piece of broken bone is sufficient, which, resting against the artery, compresses it and leads to contusion or complete rupture. The same bone can also damage the nerves passing near the artery, thereby causing necrosis and ischemic paralysis of the limb.
Failure in blood circulation disrupts the nutritional value of the muscles of the hand. As a result, muscle tissue loses its ability to contract, becomes "dry" and inelastic, and the joints of the hand are deformed, losing the ability to bend and straighten. This condition of the hand leads to serious problems with nerve tissues.
Lack of blood supply provokes irreversible processes in the nervous tissues and contributes to the active development of Volkmann's contracture.
Treatment of Volkmann's contracture
Treatment of the "clawed paw" depends on the time during which the blood circulation was disturbed and is prescribed individually based on the severity of the disease. Delay in this case can lead to irreversible consequences.
The first priority in the treatment of this disease is conservative methods. Their effectiveness and efficiency has consistently high rates and includes:
- Physical exercises aimed at developing the segment damaged by the disease.
- Exercise in water (swimming) not only improves blood flow, but has a positive effect on the development of deformed muscle tissue.
- Warm hydrogen sulfide and contrast baths.
- Electrophoresis.
- Massage.
- Manual therapy.
- Paraffin treatment with okzotert (thermotherapy).
- Magnetic pulse stimulation of the extensor muscles.
- Orthotics.
- Splinting, etc.
As a rule, the treatment of Volkmann's contracture requires a lot of time and effort. It is not worth expecting a positive result in a few weeks, since therapy can last for many years.
When a pulse in an artery is not felt, an emergency operation is performed to restore blood flow to the limb.
In extreme cases, arthroplasty of the damaged joint is performed, followed by arthroplasty to restore its mobility.
Dupuytren's contracture: what, how and why?
Dupuytren's contracture ("French disease", Dupuytren's syndrome, "trigger finger", "chicken paw", palmar fibromatosis) is a degeneration of the palmar aponeurosis, as a result of which the fingers gradually bend. Rebirth consists in thickening and shortening of the strands of the tendons of the hand, followed by the formation of scar tissue.
As a rule, the fourth and fifth fingers (ring and little fingers) are deformed, less often - the first, second and third (thumb, index and middle).
The fingers affected by fibromatosis straighten with great difficulty, and in the advanced case they do not unbend at all. You can suspect the disease if constrictions, sealing joints and nodules began to be felt in the brush.
The causes of the development of the disease are not fully understood, but there are some hypothetical factors that contribute to its appearance:
- alcoholism and smoking;
- diabetes mellitus, epilepsy, thyroid problems;
- infringement of the nerve roots;
- heredity;
- heavy vibration loads on the palms (drivers, turners, etc. are at risk).
Constant work with hands is not the root cause of the onset of the disease, it can only accelerate the development of palmar fibromatosis that has already appeared.
Treatment of Dupuytren's contracture is carried out in two ways: conservative and surgical. Choosing the type of treatment, first of all, it is necessary to determine the degree of the pathological process.
Stages of development of Dupuytren's contracture
Palmar fibromatosis is a disease that does not go away on its own and without proper treatment actively progresses and becomes more complicated. In total there are 4 stages of severity:
- 1st - the movement of the fingers is not limited in any way, but nodules are felt in the palm and strands are felt.
- 2nd - the fingers are pulled together by fibrous bands at an angle of 30 degrees or less, the motor ability is reduced.
- 3rd - the movement of the fingers is limited, the sensitivity is reduced, the bend angle is 30-90 degrees.
- 4th - fingers bent at an angle of more than 90 degrees and completely limited in movement.
Conservative treatment
Conservative therapy of Dupuytren's contracture is resorted to only at the very beginning of the disease, namely at the 1st stage. Such treatment, as a rule, does not bring curative results, but can slow the progression of the disease and slightly push back the onset of the 2nd degree.
Conservative therapy for Dupuytren's contracture at an early stage includes:
- palm gymnastics;
- physiotherapy;
- the use of splints, splints and plaster to fix the finger in an extended position without the possibility of bending;
- corticosteroid therapy, etc.
Regardless of whether conservative treatment was performed or not, the question of the need for an operation will definitely arise. Unfortunately, no way has yet been found to prevent and stop the development of hand contracture. Therefore, the only and unconditional method of treating Dupuytren's contracture is surgical intervention.
Surgical methods
To this method treatment is recommended to resort to stage 2 of the disease. If, when laying the hand on a flat table, the fingers cannot align on its surface, that is, they “become a house,” then there is a need for surgical treatment. If the fingers freely bend and unbend, then it is better to postpone the operation.
Dupuytren's contracture is not a deadly disease, but still has its own "pitfall" - a relapse.
The appearance of nodules and bumps in the palm of your hand does not mean that tomorrow the fingers may bend. This can be a long process, taking several years, during which the disease will not interfere with life in any way.
If the nodules are operated on immediately after their appearance, then a relapse can occur after the same time as the 2nd stage without surgery. For this reason, you should not rush and immediately run to the surgeon, because you can safely live, for example, 5 years with the first stage, have an operation and live another 10 years before a relapse. The total is 15 years. And an emergency operation at the initial stage will give only 10 years before a relapse and a second operation.
Surgical treatment includes two main methods:
Aponeurotomy
The method is based on dissection of the healed aponeurosis and relieving tension from the hand. The operation is performed in closed and open form.
Needle aponeurotomy (percutaneous fasciotomy)
This type of operation is performed at any stage of fibromatosis. Depending on the severity of the disease, the gradual manipulation with gradual extension of the fingers is determined.
With a needle aponeurotomy, the operation is performed closed using an ordinary medical needle. Through punctures in the skin, the needle is inserted directly into the scarring site and cuts it. One dissection is usually not enough, so they are made several at different levels of the finger and palm. This method of operation allows you to straighten your fingers to their normal state.
However, needle aponeurotomy has two serious disadvantages:
- The occurrence of relapse. Since the "problem" tissues were not removed, but only dissected, with a high probability they will continue the scarring process, leading to Dupuytren's contracture.
- Danger of nerve damage. During the operation, the surgeon releases not only the tendons from the binding scars, but also the nerves passing through them. Therefore, when performing the operation, it is important to be extremely careful not to hurt them. Damage to the nerve, fraught with a complete loss of sensation in the finger.
After percutaneous fasciotomy, the restoration of the fingers begins 2 hours after the end of the operation. In addition, the low invasiveness of surgical intervention provides a quick rehabilitation process.
Open aponeurotomy (open fasciotomy)
With an open aponeurotomy, the skin is incised in the scarring zone, followed by cutting of the damaged tissues. This method is used with a more complex degree of the disease and is more effective in comparison with the previous version of the operation.
Relapse and the risk of damage to the nerve pathways are negative components of the operation.
Aponeurectomy (aponeurectomy)
This technique is the most common and effective in the treatment of hand contracture. Aponeurectomy is an open operation during which the palm is cut and the fibrous cord is completely or partially removed:
- With partial (segmental) removal of the cord, only those areas that were subject to scarring are cut off. The aponeurosis not affected by the disease remains in the same place. This type of operation is used when total removal is impossible for some reason.
- With complete (total) removal, damaged and undamaged areas of the aponeurosis are cut out completely. The disadvantage of this operation is that even with the excision of intact areas, there is no absolute guarantee of the resumption of the disease after some.
The restoration of the flexion and extensor function of the hand after open operations to remove Dupuytren's contracture begins when the postoperative wounds heal and all sutures are removed.
Collagenase injection - a new trend in medicine
Collagenase injection is a fairly new method of conservative therapy developed and patented by American scientists. The injection is based on a special enzyme that destroys and dissolves the structure of the scar. Collagenase injection is injected directly into the aponeurosis strand and after a while the nodules and scars dissolve.
During the day after the injection, the patient is forbidden to move the brush and strain it in every possible way, that is, the arm should be in a relaxed state to avoid spreading the drug over the surrounding tissues. If the collagenase preparation enters the adjacent tissues of the arm, it is fraught with inflammation, pain and swelling.
The extension of the bent fingers should occur the next day under the strict supervision of a physician. It is forbidden to straighten your fingers at home on your own.
If the first injection did not give tangible results, a second injection of the drug is prescribed no earlier than a month later.
Within two weeks after the procedure, swelling, pain and hemorrhage can be observed at the injection site. The main complication after treatment with collagenase is relapse. Since the damaged aponeurosis is not completely removed, there is Great chance(50–80%) disease recurrence.
Treatment of contractures with folk remedies
In contrast to all diseases and ailments from time immemorial, traditional medicine has acted. No matter how many surgeons say that there is no treatment against Dupuytren's contracture, but there is only surgical therapy, people will stubbornly believe in the healing properties of the folk "first aid kit".
On the Internet you can find a lot of advice on the treatment of contractures, in which in an incredible way the flexion function of the hands is restored and here are some of them:
- Kalmyk method of treatment. The specificity of the constituent ingredients of this method stops many people from using it. The composition of the compress includes clay, sawdust and horse manure. All components must be mixed in equal proportions and applied to the diseased joint.
- Slavic method of treatment - tincture of three parts. The first is prepared from 2 tbsp. l. black poplar buds in ½ liter of vodka and infused for 10 days. The second - 1.5 tbsp. l. Mordovnik seeds pour ½ cup boiling water and wrap tightly for 4-5 hours. When preparing the third part, grate 4 tbsp. l. horseradish roots. Connect all three parts and make a compress. Leave on hand for 30 minutes and remove.
- Old copper coins. Coins are placed in a saline solution for 1 hour. To prepare the solution, dilute 1 tbsp. l. salt in ¼ liter of water. Soaked coins are applied to the sore spot of the hand for 2 days. Then a break is made for 2-3 days and the manipulation is repeated again, if after the first time there are no negative reactions in the form of green, red or blue marks on the skin.
- Pine bath. 1.5 kg of young branches of needles, pine or spruce should be boiled in 3 liters of water and left to infuse for a day. Next, ½ cup of sea salt is added to the tincture. Before use, the treatment solution can be warmed up. Reuse of the solution is not prohibited.
- Iodine-vegetable bath. Boil potato, carrot, beet and onion peels in 5 liters of water. Add to the decoction 1 tbsp. l. salt and 20 drops of iodine. Cool the iodine-vegetable mixture to 38 degrees. Pour some of the tincture into a tall container, dip your hands into it and knead them until tolerable pain for 10 minutes.
- Chestnut tincture. Grind the chestnuts and fill a half-liter jar with them so that 3 cm remains free to the top. Pour the chestnuts ammonia and leave to infuse for 9 days in a dark place. Apply as a rub for 2 months.
Of course, the treatment of complex diseases such as Dupuytren's contracture or Volkmann's contracture cannot be blindly trusted traditional medicine, the more medical experience has shown more than once that in some cases they can be cured only by surgery.
Be vigilant and careful with your health, because it is unique.
How to forget about pain in the joints?
- Joint pain limits your movement and life...
- You are worried about discomfort, crunching and systematic pain ...
- Perhaps you have tried a bunch of medicines, creams and ointments ...
- But judging by the fact that you are reading these lines, they did not help you much ...
Contracture of the fingers: treatment
Contracture of the fingers is a position of the hand, in which there is a shortening of the tendons of the palmar surface. Over time, cicatricial degeneration is observed, and in this case, the hand loses its motor function. The process itself proceeds painlessly, but when you try to move the affected joints, a severe pain syndrome develops.
Some neurohumoral features of the body contribute to the fact that predominantly contracture of the fingers develops in middle-aged men. Causes of the development of the pathological process: from systemic diseases of the connective tissue (Dupuytren's contracture) to traumatic lesions of the hand.
The pathogenesis of the development of contracture lies in the fact that under the influence of various causes, afferent impulses in the nerve endings of the hand are transformed, as a result of which strands, nodules and scars begin to form. There is a shortening of the palmar fascia and a thickening of the lower parts of the joints of the fingers.
With the progression of the disease, the contracture of the fingers begins with the metacarpophalangeal joints, then the interphalangeal joints are affected. As a result, a dense cord stretches from the beginning of the palm to the fingers, limiting the movement of the hand.
Flexion contracture of fingers
Flexion contracture of the fingers, depending on the location of the strand, can be classified as:
According to the degree of limitation of the contracture of the fingers, the Tubian classification is used:
- first degree, finger flexion up to 30 degrees;
- the second degree - up to 70 degrees;
- third degree - up to 90 degrees;
- fourth degree - up to 135 degrees.
The peculiarity of this pathology is that both hands are more often affected. The clinical picture is typical, the hand loses its function, over time, bedsores, inflammation and maceration of the skin appear.
In young people, contracture is more malignant and can develop over 3-5 years.
Treatment of finger contact
Conservative treatment of contracture of the fingers is carried out only at the initial stage and is aimed at preserving the function of the hand as long as possible. For this, several groups of drugs are prescribed:
- vascular;
- normalizing rheological properties of blood;
- in some cases, it helps to restore the hormonal status of the body;
- vitamins of group E;
- nootropic drugs.
It is mandatory to carry out physiotherapy with applications, paraffin baths, phonophoresis, shock wave therapy, massage, exercise therapy, reflexology.
Surgical treatment of contracture of the fingers is a technically complex operation, which does not always lead to a positive result. Unfortunately, there is a high chance of recurrence.
Surgical interventions are carried out in the presence of a second degree or higher contracture, with a recurrence of the process, with a loss of hand performance. Relatively speaking, all types of operations can be divided into:
- Palliative - that is, during the procedure, only the scar tissue itself is excised. Such operations are more gentle for the patient, but the percentage of recurrence is quite high.
- Radical operations - excision not only of scar tissue, but of the aponeurosis of the palm itself. The prognosis for such interventions is favorable and virtually eliminates the recurrence of the process.
Exercise therapy for contracture of the fingers
After surgery or with conservative management of patients, doctors must prescribe exercise therapy for contracture of the fingers. Exercises can be carried out at home, but the complex must be selected by a physiotherapist or exercise therapy doctor.
The fact is that with improper physical education, the desire to unclench the “closed” fingers with force, you can only harm yourself more. Therefore, a specialist selects a set of exercises, shows how to perform it correctly, and only after that it is possible and necessary to regularly carry out such exercises for the brush.
Why should you come to us?
- Our clinic is multidisciplinary, thanks to which our specialists have the opportunity to conduct a comprehensive examination of the body to identify the cause of the development of contracture of the fingers.
- The International Surgical Center employs highly qualified doctors who use the latest endoscopic techniques for the surgical treatment of contractures.
- Equipping operating rooms with modern equipment allows minimizing the risks after operations and reducing the likelihood of recurrence.
- We create an individual treatment plan for patients by combining various methods.
A stable limitation in the mobility of a joint is called a contracture. Physiology is based on the occurrence of inflammatory and pathological changes in soft tissues, tendons, mimic and other muscles. Classification is associated with the causes and nature of impaired mobility of the joints of the legs, arms and face.
According to the International Classification of Diseases 10th revision (ICD-10), the ICD 10 code is assigned - M24.5. There are contractures with other dedicated ICD-10 codes. It most often affects the most active joints - the knee, elbow, temporomandibular joint (TMJ).
Physiology, occurrence and types of contractures are still being studied. The classification divides them into congenital and acquired joint pathologies. Congenital appear due to malformations of muscles, joints (congenital clubfoot, torticollis).
Acquired pathologies, in turn, are divided into several types:
- Neurogenic - occurs when there are disorders in the central or peripheral nervous system. There is a violation of the facial functions of the face (TMJ), innervation of other organs.
- Myogenic is characterized by pathological changes in muscles, leading to atrophic processes. The extensor function is often impaired.
- Desmogenic contracture is associated with wrinkling of the fascia and ligaments.
- Tendogenic appears with damage and inflammation in the tendons.
- Arthrogenic - the consequences of pathological processes of the joint.
- Immobilization contracture appears after a long immobilization of the injured limb after an injury or surgery, anesthesia.
Often in practice there are mixed types. This is due to the fact that the contracture of a certain type that has arisen leads to disruption of the normal nutrition and blood supply to the affected joint, and other pathological processes join over time.
The physiology of the process of joint damage differs in primary and secondary. The primary process is limited to the affected joint. Secondary contracture involves a healthy adjacent joint in the process. 
The general classification is divided into flexion, extensor, adductor and abductor. There is also a rotational joint pathology that disrupts rotational movements,.
Etiology of the disease
Based on the above types and types, it can be determined that there are many causes that can cause joint contracture. The term itself is essentially a symptom, meaning a restriction in the movement of the joint. Despite this, he is assigned a separate ICD-10 code. Therefore, a pathological process may occur after a disease, injury, anesthesia or congenital anomaly.
The resulting mechanical damage is the occurrence of post-traumatic contracture. It can be a dislocation, a bruise, a fracture, and even a burn. The formation of a scar reduces the elasticity around the joint tissue and makes it difficult for the joint to move.
A similar effect is exerted by degenerative-inflammatory processes of bones and joints. Damaged nerve fibers and muscle tissue also have a negative impact on the normal functioning of the joint.
A period of prolonged limitation of the functions of certain parts of the body due to the imposition of a cast, splints or anesthesia causes immobilization contracture. Depending on the recovery period during post-traumatic immobilization, the severity of the process is revealed.
A disease such as contracture of the lower jaw of the face (TMJ) is quite common due to the fact that the muscles and joints of the face are constantly in motion. The function of the mimic muscles of the face is almost constant.
The contracture of the lower jaw is a consequence of pathological changes in the properties of soft tissues (decrease in elasticity). The natural functions of the mimic and chewing muscles of the temporomandibular joint are disturbed. Unstable contracture occurs with inflammatory diseases of the lower jaw of the face, mimic muscles and after prolonged use of the splint. Persistent contracture occurs after facial injuries, anesthesia during dental procedures, with injury to the facial muscles. The period of immobilization affects the development of the disease and the state of facial muscles. According to ICD-10, it refers to other diseases of the jaws.
Symptoms of contracture of the lower jaw are based on difficulty eating, impaired function of facial muscles, speech. A person feels such a feeling as after anesthesia at the dentist.
Treatment of contracture of the lower jaw of the face (TMJ) is performed using surgical methods. The resulting scars are dissected, which leads to the return of normal function of facial muscles and chewing activity. Of particular importance is the recovery period after surgery, which includes therapeutic exercises, physiotherapy. 
Hand lesion
Volkmann's contracture is manifested by a stable limitation of hand mobility. The hand begins to resemble the clawed paw of an animal. The hand on the left is less affected than the right.
Volkmann's ischemic contracture is characterized by rapid development and affects the joints of the shoulder and forearm. It has the number M62-23 according to ICD-10; M62-24. The condition can provoke pain associated with trauma to the joints of the hand. There is a violation of innervation and motor activity, a feeling, as after anesthesia.
Physiology is based on the violation of both extensor and flexion functions. The position of the brush is constantly in a bent state and motionless. The consequence of the pathological process is a violation of blood supply due to a fracture or dislocation in the elbow, shoulder joint. Prolonged clamping bandage can also lead to contractures.
Main symptoms:
- type of clawed paw;
- difficulty in normal hand movement;
- violation of innervation (condition, as after anesthesia);
- brush deformity.
 The period of impaired blood supply affects the course and consequences of the disease. If this is due to objects or bandages compressing the surface, then the immediate release of the hand is necessary. In a post-traumatic condition, treatment is aimed at stopping further pathological processes and partially maintaining normal muscle function. Operative methods of treatment using anesthesia are also allowed.
The period of impaired blood supply affects the course and consequences of the disease. If this is due to objects or bandages compressing the surface, then the immediate release of the hand is necessary. In a post-traumatic condition, treatment is aimed at stopping further pathological processes and partially maintaining normal muscle function. Operative methods of treatment using anesthesia are also allowed.
Volkmann's ischemic contracture requires an individual approach to healing. Conservative methods, such as physiotherapy exercises, physiotherapy, gentle massage, are quite effective. A positive effect gives a recovery period, including spa treatment with the use of compresses, hydrogen sulfide baths, mud treatments.
Palmar fibromatosis
In practice, Dupuytren's contracture is quite common - a disease that leads to deformation and disruption of the normal function of hand movement. It has a separate code according to ICD-10 M72.0. The ring finger and little finger are often affected. Dupuytren's disease is not fully understood and refers to chronic forms of the course.
Due to degenerative-inflammatory processes, wrinkling of the tendons of the palm occurs and the extensor ability of the fingers is disturbed. 
Dupuytren's contracture is characterized by three degrees of severity, characterized by a violation of sensitivity and the severity of the motor function of the joints. With the progression of the process, there is an increase in soreness and stiffness of the joints and muscles.
Due to the fact that predisposing factors are not precisely established, Dupuytren's contracture often occurs with concomitant diseases. One example is scleroderma (spotted idiopathic atrophoderma).
Idiopathic atrophoderma is prone to affecting young girls under 20 and children. One of the stages of the disease is the defeat of the small joints of the legs and arms. It is characterized by such a symptom as Dupuytren's contracture. Children have a combination of diseases such as Raynaud's syndrome, idiopathic atrophoderma and Dupuytren's contracture.
The treatment algorithm for Dupuytren's disease is determined by the orthopedist. In mild stages, conservative therapy is prescribed. Used to restore normal joint function surgical treatment using anesthesia.
Finger contracture
Weinstein's contracture according to ICD-10 is included in the M24 group. Associated with an injury to the upper part of the finger. The cause of the occurrence is a post-traumatic condition, after a direct blow to the finger.
With timely treatment does not pose a threat. But when delayed with a trip to a medical facility, it threatens the process of deformation and a violation of the motor activity of the injured finger and its muscles.
Arthrosis of the elbow joint is a pathological condition that is caused by degenerative changes in the area of the epicondyles of the shoulder. It is not as common as arthrosis of other joints, but a rather dangerous disease.
Based on the International Classification of Diseases in the 10th revision (ICD-10), arthrosis of the elbow joint belongs to the group of diseases of the musculoskeletal system and connective tissue. The disease was assigned the M19 diagnosis code according to ICD-10 and is divided into the following groups:
Post-traumatic arthrosis with localization in the shoulder (ICD-10 code - M19.12), forearm (according to ICD-10 - M19.13).
Osteoarthritis of other joints is primary with localization in the shoulder (ICD-10 code - M19.02) and forearm (M19.03).
Secondary arthrosis (ICD-10 code - M19.22 - 19.23).
Another unrefined with localization in the shoulder and forearm (ICD-10 code - M19.82-19.83).
Arthrosis unrefined (ICD-10 code - M19.92-19.93).
The elbow joint is quite mobile and rarely undergoes inflammatory processes. Therefore, the most common causes of pathological conditions are injuries or professional "hazards" associated with a long forced position of the hand.
Symptoms
The main symptoms characteristic of elbow arthrosis are manifested in the occurrence of pain and cause a violation of the mobility of the arm. The nature and frequency of clinical manifestations depends on the stage of joint damage. In total, it is customary to distinguish three degrees of the disease, depending on degenerative and structural changes in the structure of the elbow.
In order to distinguish arthrosis of the elbow joint from other diseases of the joints of the hands with characteristic signs, special diagnostic techniques were identified.
Thompson's symptom is based on the inability to keep the hand in a compressed position during dorsiflexion. The hand quickly moves into the position of palmar flexion.
The second way to identify arthrosis is a positive symptom of Welt. It is necessary to bend both arms at the same time. A healthy hand performs this procedure faster. During the two methods of diagnosing, the whole process is accompanied by painful sensations. 
1 degree
The first degree is characterized by the weakest manifestations of the disease. There are still no visible structural changes in the joint, so the clinical picture is based on rare periods of exacerbations and long-term remissions.
Symptoms in the form of pain appear only after physical exertion on the affected arm. They are small and tolerable. Externally and on palpation, it is almost impossible to determine deviations. There may be a feeling of discomfort with sudden movements of the hand or during the flexion-extension process. Treatment is still quite effective in this condition.
2 degree
If the disease is not treated, then in the second degree arthrosis of the elbow joint begins to progress, the tissue deforms, structural changes are observed radiographically. The feeling of pain is greatly enhanced and can occur even during rest.
Symptoms such as dry crunch in the elbow, atrophy of the muscles of the arm, impaired mobility of the arm and the inability to take it back are added.
It is at the second degree of development of the disease that the patient realizes that treatment is necessary, and most often seeks medical help.
Working capacity is disturbed, painful sensations are expressed quite clearly, reaching the area of the shoulder girdle. 
3 degree
In the third degree, rather severe aching pains appear, which can occur at any time of the day. Motor activity is limited not only to the elbow, but also to the shoulder joint. Symptoms in the form of pain subside only during the fixation of the hand in a forced position. In addition, even changes in the weather or a change in the climatic zone can provoke an attack of pain.
This degree is considered a neglected condition, leading to the destruction of cartilage and strong bone growth, which is not characteristic of a healthy state. Visually, it can be seen that the affected arm becomes somewhat shorter than the healthy one. With a 3 degree of damage, a medical advisory commission may prescribe a disability associated with a limitation of a person’s physical capabilities, guided by a diagnosis according to ICD-10 - arthrosis.
Treatment of arthrosis
Treatment requires an integrated approach and monitoring of a patient with arthrosis. Regardless of whether it is post-traumatic or age-related arthrosis, immobilization of the injured hand is required. This measure allows you to stop the process of further destruction of the joint due to physical activity.
To treat such arthrosis, it is necessary to prescribe a sparing regimen. Temporarily you need to refrain from physical activity during treatment. It is recommended to follow a diet limiting the consumption of fatty and spicy foods, products made from yeast dough, and reduce the amount of salt. 
There are 4 main areas of treatment:
- Medical therapy.
- Physiotherapy and exercise therapy.
- Surgical intervention.
- Therapy with folk remedies.
Medical treatment is the most common. With the first degrees of the disease, it makes it possible to achieve good results. The appointment of non-steroidal anti-inflammatory drugs intramuscularly or in tablet forms is shown. Intra-articular administration of these drugs is also effective.
Chondroprotectors are the main component of the medicine in the treatment of arthrosis, such as shoulder, knee, elbow and other joints. It is they who restore cartilage tissue, allow you to cure the disease. They are used in the form of tablets, ointments, powders.
For a positive effect after the removal of the exacerbation of the disease, treatment with physiotherapy is required. Electrophoresis sessions, laser therapy, body wraps, warming up are prescribed. In the recovery period, a course of massage and, if desired, manual therapy is carried out. Self-administration without consulting a doctor is contraindicated. 
Physiotherapy exercises and gymnastics are on a par with drug therapy in the process of healing. Classes for the muscles of the shoulder girdle and arms are selected individually by the doctor so as not to harm the joint. You should be especially careful with exercises in situations where post-traumatic arthrosis. It must be ensured that the procedures will not harm the patient.
Treatment with folk remedies is aimed at enriching bones and joints with collagen, strengthening overall immunity and alleviating painful symptoms. Compresses, baths, rubbing the joints are popular.
Combining classical medicine and using folk ways treatment, you can reduce the time of recovery and reduce the negative consequences in the future. Therefore, having the slightest suspicion of arthrosis, one should not delay consulting a doctor.
Gouty arthritis ICD code 10
A disease that develops due to the deposition of uric acid salts in the joints and organs. This happens when metabolism is disturbed in the human body and uric acid crystals (or urates) are deposited in the kidneys and joints. This leads to inflammation, difficulty in movement, and deformation of the joint.  The kidneys also suffer, in which crystals are deposited, which disrupts the normal functioning of the excretory system. There is a classification of diseases, which lists all the names and categorized by development, treatment, clinical picture. This classification is called the ICD (International Classification of Diseases). Gouty arthritis ranks under the name ICD 10.
The kidneys also suffer, in which crystals are deposited, which disrupts the normal functioning of the excretory system. There is a classification of diseases, which lists all the names and categorized by development, treatment, clinical picture. This classification is called the ICD (International Classification of Diseases). Gouty arthritis ranks under the name ICD 10.
Gout and gouty arthritis and their place in ICD 10
When a patient comes to a medical facility and is diagnosed with gouty arthritis, ICD code 10 is written on a card. This is done so that the doctors and the rest of the staff understand what the patient's diagnosis is. All diseases according to the ICD classification are clearly divided into their groups and subgroups, where they are indicated by letters of the alphabet and numbers, respectively. Each group of diseases has its own designation.
Also, there are generally accepted norms of therapy, as a single main criterion, tactics or method of treatment that is prescribed to all patients with a particular disease. Further, judging by the patient's condition, the development of the disease or other concomitant pathologies, he is prescribed symptomatic therapy.
The entire classification of diseases of the musculoskeletal system in the ICD is located under the letter M, and each type of such pathology is assigned its own number from M00 to M99. Gouty arthritis in the ICD is in place of M10, in which there are subgroups with designations for various types of gouty arthritis. This includes:
- Gout, unspecified
- Gout associated with impaired renal function
- Medicinal
- Secondary
- lead
- idiopathic
When a patient contacts a medical institution, a detailed history is taken, laboratory (analyzes) and instrumental methods (X-ray, ultrasound, and so on) study the disease. After an accurate diagnosis, the doctor sets the ICD 10 code and prescribes the appropriate treatment and symptomatic therapy.
Cause of gouty arthritis according to ICD 10
It has been proven that gouty arthritis most often affects men and only at the age, and women, if they get sick, only after menopause. Young people are not exposed to the disease due to the fact that hormones, of which a sufficient amount is released in young people, are able to remove uric acid salts from the body, which does not allow crystals to linger and settle in the organs. With age, the amount of hormones decreases due to the inhibition of certain body processes and the process of removing uric acid no longer proceeds as intensively as before. 
But, nevertheless, until now, scientists cannot accurately name the reason why gouty arthritis occurs. According to statistics and the study of the disease, risk factors are identified that can give impetus to the development of the pathological process of accumulation of uric acid in organs. These are risk factors such as:
- Heredity. Many types of chronic inflammatory joint pathologies are inherited. It may be that the disease does not manifest itself in a person’s entire life, but this is extremely rare.
- Diseases are precursors. Renal pathologies, heart disease, hormonal disorders.
- Incorrect or inadequate nutrition. Abuse of meat or offal, strong tea and coffee, alcohol, chocolate.
- Long-term use of certain medications. Such as means for lowering pressure, cytostatic and diuretic.
In addition, there are primary and secondary gout. Primary occurs when a combination of genetic heredity and the use of large quantities of unwanted products. Secondary develops with cardiovascular diseases, hormonal disorders and intake medicines. The difference in the occurrence of the disease does not affect the clinical picture of the manifestation of symptoms, the whole point is how exactly gouty arthritis developed, which organs and mechanisms it affected, in order to assess at what stage the pathological process is. If necessary, explain to the patient why the disease began, and how exactly to correct the lifestyle in order to remove an additional factor provoking the disease.
Classification of the disease in ICD 10
There is a large variety of gouty arthritis in connection with clinical symptoms, the pathogenesis of the disease, the mechanism of uric acid deposition, the manifestation of articular forms of gouty arthritis. 
Primary and secondary gout differ in the mechanism of development of the disease. According to the different mechanism of accumulation of uric acid crystals, gout can be of different types:
- hypoexcretory;
- Metabolic;
- Mixed type.
According to the clinical picture of the course of gouty arthritis, it differs:
- Asymptomatic manifestations of the disease;
- Acute form of gouty arthritis;
- Development of tophi;
- Pathologies of the kidneys that have developed against the background of gout.
According to the manifestation of articular forms, there are:
- acute form;
- Intermittent form;
- The chronic form is manifested by the deposition of tophi.
Gouty arthritis and its other types and manifestations are listed in ICD 10 and each form of the disease is assigned its own, personal number.
Gouty arthritis and its clinical manifestations
The disease has one peculiar negative quality, which is that the accumulation of uric acid crystals can occur unnoticed by the patient. Gouty arthritis does not show any symptoms, there is no clinical picture, but if there is a strong stressful situation, a serious illness, this can give impetus to the development of the disease. In this regard, a rather vivid clinical picture develops, since the amount of deposited uric acid in the organs is large and gouty arthritis, as it were, “is on pause” and is waiting for the moment for rapid development.
There are three stages of the disease, differing in the number of symptoms and the severity of the course.

Gouty arthritis does not affect large joints, being localized in small ones. Most often it is the joints of the legs and hands. In 9 out of 10 cases, the joint of the big toe is affected first. The first manifestations of the disease are always pronounced and the person begins to worry and seek help from a medical institution.
During a vivid pathological process, the symptoms are extremely specific. There are severe pains, inflammation, swelling, redness, fever at the joint site. Uric acid crystals are deposited in the cavity and on the surface of the joint, as well as under the skin. If the course of an acute attack is long, then the decaying tissues of the joint, together with uric acid, form tophi (nodules). In places where there is no joint tissue, it is replaced by urates, which leads to a decrease in functioning and to a strong modification of the limb. Gradually, the joint becomes unable to do its job and the person becomes disabled.
In women, the gouty form rarely causes such strong changes in the joint, even less often tophi are formed, so the disease does not cause significant deformity and loss of joint function. In men, on the contrary, the gouty form is extremely aggressive and if no measures are taken to eliminate the disease, the person becomes disabled.
Diagnostics
Hyperurinemia in a laboratory blood test is not a reliable sign confirming gouty arthritis. This may indicate a metabolic disorder in the body and not manifest itself in the articular form. During an acute attack, a joint (or tophi, if any) is punctured and the material obtained is analyzed in the laboratory, in which white crystalline deposits of uric acid are found. 
When an attack of gouty arthritis occurs, it is quite difficult to determine what kind of inflammatory process is present at the moment. Since the symptoms are similar to other chronic diseases of the articular tissue.
X-ray examination, with a long course of an acute attack, allows us to differentiate the pathology in connection with the detection of joint destruction on the radiograph, the presence of punches (places where the joint tissue has undergone decay).
Basic Treatments
There are three main areas, according to ICD 10:
- Medical. NSAIDs are prescribed to reduce pain and inflammation, glucocorticoids - regulate the hormonal background of the body, colchicine - lowers the temperature, stops the processes of crystallization of uric acid and its production, which significantly affects the inflammatory process already at an early stage of an attack of gouty arthritis.
- Physiotherapy. Treatment is aimed at local reduction of inflammation, pain, swelling and temperature. Methods such as electrophoresis medicines allow the drug to locally penetrate into the tissues and intensively perform its work. Applications to the site of injury (for example, using dimexide) also increase the chances of a speedy recovery and getting rid of a number of symptoms during an acute attack.
- exercise therapy. It is aimed at improving the mobility of the articular apparatus and the restoration of partially lost mobility due to the combination of a drug treatment method, physiotherapy and physical education. Developed special exercises, allowing you to gradually increase the load during classes, which over time makes it possible to fully restore all lost functions.
For example, foot exercises:

Prevention and prognosis of the disease
Gouty arthritis can be prevented, it is enough to monitor your diet, limit alcohol consumption to acceptable doses. Engage in physical education or do daily morning exercises. It's quite simple, but effective. 
The prognosis is quite positive, but only on condition that the patient makes a lifestyle correction, which will prevent the manifestation of acute attacks of the disease and reduce it to a long period of remission.
Outcome
Gouty arthritis according to ICD10 is a systemic disease associated with metabolic disorders. This can be avoided by taking care of your health, nutrition and moderate physical exercise on the body.
Many joint diseases are accompanied by limited mobility of the limb, the inability to perform the simplest movements. Contracture of the elbow joint occurs for various reasons, and with a combined form, movement is limited in any direction.
What?
The elbow joint is a complex articulation, therefore it is often subjected to various injuries.
In a healthy person, the arm at the elbow bends and unbends without problems. If a person bends the arm, then the elbow is at an angle of 40 degrees, and when unbending - at 180. You can turn the arm back, rotate and turn the forearm.
The contracture of the elbow joint is a partial or complete restriction of the function of the range of motion. Difficulties can occur with a certain type of movement, for example, when flexing or unbending. With a combined form of pathology, the hand becomes almost lifeless.
Causes
Factors that provoke contracture:
- congenital pathologies in the form of underdevelopment of bone tissue, shortened muscle fibers, altered structure of muscle tissue;
- the presence of scars in the joint cavity, formed after the inflammatory process, or in the post-traumatic period;
- violation of the integrity of articular tissues;
- proliferation of connective tissue, which begins to replace the muscle tissue of the joint, and it becomes impossible to bend the arm;
- joint injuries, which include fractures, dislocations. Any traumatic injury. Elbow contracture after a fracture is common;
- gunshot wound;
- problems with blood flow;
- severe burns;
- abscess;
- diseases of the nervous system;
- arthritis occurring in a purulent form;
- hysterical psychosis.
Elderly patients are diagnosed with a post-traumatic type of contracture.
The post-traumatic type of pathology is more often caused by unsuccessful falls on the elbow, bruises, circulatory problems, pathological loss of elasticity of soft tissues.
Classification of contractures
Post-traumatic contracture is classified as follows:
- Stage 1 occurs a month after the injury. Limited movement occurs after motor fixation, pain. The psychological factor also influences the development of the phenomenon. If you seek medical help at the initial stage, then the problem is easily eliminated;
- Grade 2 contracture can develop when more than a month has passed since the injury to the joint. It is difficult to make basic movements due to the formation of adhesions and scars;
- Grade 3 contracture manifests itself several months after the injury to the joint. During this time, the scars on the flexor muscle degenerate into fibrous tissue and contract, which leads to limited mobility.

Elbow flexion contracture is classified into 4 stages:
- 1 degree. You can straighten your arm at the elbow no less than 170 degrees;
- 2 stage. The extension angle decreases from 170 to 130 degrees;
- Stage 3 is characterized by an extension angle of 90 to 130 degrees;
- Grade 4 is the most severe. It is possible to extend the extension less than 90 degrees.
With flexion contracture, extension of the limb is limited, with extensor contracture, flexion. Flexion contracture is the most common.
What the joint looks like with contracture can be seen in the photo.
Diagnosis of contractures
To confirm the diagnosis and prescribe the correct treatment for contracture of the elbow joint, a comprehensive diagnosis is prescribed, consisting of the following measures:
- X-ray examination to study the state of cartilage and bone tissue;
- Computed tomography or MRI to examine the internal articular tissues and detect articular changes in them;
- Laboratory blood tests.

After the above procedures, additional diagnostics may be required if the contracture is caused by neurogenic factors.
When making a diagnosis, ICD10 is used - the International Classification of Diseases. Under the code M24.52 there is a contracture in the shoulder area. These are the humerus and elbow joint.
Post-traumatic type of contracture of the elbow according to ICD10 goes under the code M24.5 and refers to acquired deformities, denoted by the code M20-M21.
Treatment
For contracture of the elbow joint, the traditional method of treatment is usually used. Conservative treatment is effective with timely access to a doctor and consists of the following procedures:
- the imposition of plaster bandages that correct the position of the joint;
- physiotherapy;
- thermal physiotherapy procedures;
- massage;
- stretching technique.
With active medical procedures, pain may be disturbing during treatment. Therefore, in order to avoid additional inflammation of the joint tissues, they begin to be treated with medicines from the group of non-steroids. These are drugs with analgesic and anti-inflammatory effects. With severe pain, blockade of the elbow joint is indicated.
For the treatment and prevention of DISEASES OF THE JOINTS and SPINE, our readers use the method of fast and non-surgical treatment recommended by the leading rheumatologists of Russia, who decided to oppose pharmaceutical lawlessness and presented a medicine that REALLY TREATS! We got acquainted with this technique and decided to bring it to your attention.
In case of detection of massive scar tissue in the connective apparatus of the elbow joint, the problem is treated with surgical intervention in the form of arthroscopy. Surgery is also prescribed in cases where the traditional technique has not been able to eliminate the limitation of movements.
An effective surgical method for contracture is arthrolysis of the elbow. During arthrolysis, the articular cavity is opened, then a part of the connective tissue that prevents the normal motor activity of the limb is excised.

After excision of scars during arthrolysis, the affected tissues are replaced with implants.
If the entire connective tissue is affected by scars, then joint arthroplasty is indicated.
If contracture began to develop against the background of a fracture and subsequent malunion of the bones, then surgical intervention is indispensable. Before the operation, a number of activities are carried out. These are physiotherapy sessions, special exercises for exercise therapy, intra-articular injections that help eliminate signs of contracture. Such an integrated approach to the operation allows to reduce the time of the rehabilitation period, and also prevents the development of negative consequences after the operation.
With the neglected nature of the elbow contracture, which lasted for a long time, if the surgical intervention is not performed, the patient may remain disabled.
In the case of timely treatment, both conservative and surgical methods give a favorable outcome. Therefore, with the appearance of signs of pathology, it is important to seek medical help in time.
Physiotherapy
Physiotherapy procedures are included in the complex conservative treatment for limited joint mobility. Physiotherapy gives the following results:
- Improves blood supply to the joint. The tissues receive the necessary amount of oxygen and nutrition.
- Scars dissolve faster.
- The puffiness goes away.
- Stops the inflammatory process.

The following types of physiotherapy procedures are prescribed:
- electrophoresis with nonsteroidal drugs to relieve pain and stop the inflammatory process. With electrophoresis, drugs from the group of corticosteroids and analgesics can also come to the joint;
- magnetic therapy;
- laser treatment;
- shock wave procedures;
- applications with paraffin and ozocerite;
- balneological procedures.
Physiotherapy is effective at the initial stage of the course of the elbow contracture. During this period, galvanization procedures are shown, when a low frequency current is applied to the diseased area. With a timely visit to the doctor, several sessions of galvanization are enough to eliminate the problem.
Massage
For the treatment and subsequent development of the elbow joint, massage sessions are included in the complex treatment.
Benefits of massage for contracture:
- blood flow stabilizes. Tissues receive the right amount of nutrition and oxygen;
- eliminates swelling in the elbow area;
- pain disappears;
- improves overall health and mood.
After each massage session, the injured hand should be at rest. Any overexertion for a diseased limb is prohibited.
Massage sessions are performed when the patient is in a lying or sitting position. Stroking and squeezing movements are used.

Massage starts from the area above the shoulder. First comes stroking, squeezing and kneading, then shaking manipulations. Movements are directed from the elbow joint to the shoulder joint, affecting all the muscles of the shoulder girdle.
Massage sessions are carried out in a sparing mode. Painful and other uncomfortable movements are excluded. Carefully massaged areas at the site of attachment of the tendons.
The duration of the session depends on the stage of contracture and the size of the elbow joint. Massage goes well with thermal procedures and therapeutic exercises.
How to forget about joint pain forever?
Have you ever experienced unbearable joint pain or constant back pain? Judging by the fact that you are reading this article, you already know them personally. And, of course, you know firsthand what it is:
- constant aching and sharp pains;
- inability to move comfortably and easily;
- constant tension of the back muscles;
- unpleasant crunching and clicking in the joints;
- sharp shooting in the spine or causeless pain in the joints;
- inability to sit in one position for a long time.
Now answer the question: does it suit you? Can such pain be endured? And how much money have you already spent on ineffective treatment? That's right - it's time to end this! Do you agree? That is why we decided to publish, which reveals the secrets of getting rid of pain in the joints and back.
20666 0
Contracture - limitation of passive movements in the joint - is one of the most common complications in hand surgery. A particularly acute problem is the treatment of patients with post-traumatic contractures of the metacarpophalangeal joints (PFJ). Being spherical in shape, PPS provide movement of the fingers in the most important sector. According to R. Kosh, the loss of this ability leads to a decrease in the functionality of the hand by 40-66.5%.
Etiology and pathogenesis
All contractures can be divided into primary and secondary.Primary PFJ contractures occur due to direct (primary) damage to the tissues that form the joint. By their origin, they can be arthrogenic (after intra-articular fractures) and desmogenic (after damage to the ligaments and joint capsule) (Scheme 27.10.1).
Scheme 27.10.1. Pathogenesis of primary post-traumatic contractures of PFS.
The processes of scarring of the joint capsule and (or) the formation of scars between the articular surfaces that develop after injury block the movements of the main phalanx. Subsequently, secondary changes in the intact sections of the joint capsule, and their wrinkling due to long-term limitation of function, may join this.
Primary contractures differ in that, firstly, they form quickly (during the first 4-6 weeks after injury). Secondly, primary contractures are difficult to treat. The more pronounced the damage to the elements of the PFC, the worse the prognosis for the function.
Secondary contractures develop after trauma to tissues located outside the PFS, when tendons, muscles, nerves, or skin are damaged, and the joint itself remains intact (Scheme 27.10.2).

Scheme 27.10.2. Pathogenesis of secondary post-traumatic contractures of the metacarpophalangeal joints (explanation in the text).
As a result of trauma and (or) surgery, an extra-articular blockade of the kinematic chain occurs with fixation of the main phalanges in a certain position and restriction of the sector of movements.
It is important to note that at this stage, the contracture is false, since all elements of the PFS remain normal, and after the elimination of extra-articular causes of movement in the joint, they are immediately restored in full.
However, with the long-term existence of false contracture, secondary degenerative-dystrophic changes gradually develop in the PFS capsule, as a result of which its relaxed sections contract, limiting the range of passive movements in the joint. There is a relatively persistent restriction of movement in the PFS, which is no longer fully eliminated after the elimination of the extra-articular causes that caused it. This contracture can be called true and requires special treatment, which involves a direct effect on the articular structures.
It is important to note that, unlike primary contractures, secondary contractures develop more slowly, sometimes over many months and even years.
From a practical point of view, the process of development of true contracture can be divided into two periods: unstable and persistent contractures. Unstable contractures are distinguished by the fact that with appropriate efforts (for example, after a session of mechanotherapy in combination with thermal exposure), the range of motion in the joint is restored, but then again limited. In these cases, conservative treatment quickly gives a good and stable result.
With persistent contractures, conservative treatment is also able to increase the range of motion to some extent, but not always. In most cases, the chances of a significant improvement in function are given only by surgical treatment.
The rate of development of secondary contractures increases significantly when a neurodystrophic syndrome develops in the post-traumatic period with trophoneurotic changes in tissues in the form of edema, cyanosis, sensory disturbances and pain.
Depending on the sector of restriction of movements, contractures are flexion (when the proximal phalanx is fixed in the flexion position and therefore the extension sector is limited), extensor (when the main phalanx is in the extension position, and the flexion sector is limited) and combined. The greatest loss of finger function occurs with extensor contractures, since in this case the most important (flexion) sector of movements suffers (Fig. 27.10.1).

Rice. 27.10.1. Location of the sector of lost finger movements (shaded) in flexion (a) and extensor (b) contractures of the PJC (explanation in the text).
The most common are extensor contractures, since it is in this position that inexperienced surgeons fix the hand during injuries and after operations. The frequent development of extensor contractures is determined by the peculiarities of the anatomical structure of the PFS, among which the most important are the relaxation of the collateral ligaments during extension and their tension during flexion. A long stay of the PPS in the position of full extension in the joint leads to a persistent shortening of the ligaments, therefore, when trying to bring the fingers into the flexion position, the ligaments that have lost their elasticity prevent the bending of the main phalanges.
It is important to note that with a long-term extensor contracture, not only the relaxed dorsal parts of the capsule and collateral ligaments are shortened, but also the skin covering the dorsum of the joint. Its elasticity decreases sharply, therefore, when the main phalanges are bent, the skin is stretched, its area above the head loses blood supply and can become dead if this position is maintained for a long time. All this is taken into account when choosing a treatment method.
Choice of treatment for contractures
The choice of treatment method depends on the type of contracture and its severity (Scheme 27.10.3).
Scheme 27.10.3. The choice of treatment method for various types and degrees of development of contractures of the metacarpophalangeal joints (explanation in the text).
Primary arthrogenic contractures. With an injury to the articular surfaces and the formation of cicatricial adhesions between them, the prognosis for the function is poor, since even scars stretched as a result of treatment are again reduced and movements in the joint are again limited. That is why arthroplasty - the operation of modeling articular surfaces with the removal of cartilage and bone tissue - as a rule, does not give a good result.
Endoprosthesis replacement of joints is also not widely used due to the lack of adequately reliable prostheses, as well as the presence in the vast majority of cases of concomitant damage to the periarticular tissues and capsular apparatus.
Transplantation of blood-supplied small joints from the foot is possible, including the inclusion of the tendon apparatus into the complex of tissues. However, the need to revascularize the graft by applying microvascular anastomoses makes this operation complicated and expensive. In addition, practice has shown that these interventions allow only a very limited range of active movements in the transplanted joint. This makes the indications for this method of treatment very relative.
In general, in clinical practice, surgeons are often forced to stabilize the fingers by arthrodesis of the joints.
Primary desmogenic contractures.
A fundamentally different situation arises in cases where the articular surfaces are preserved, and the restriction of mobility is associated with damage and cicatricial changes in the capsule and collateral ligaments of the PFS.
Depending on the severity of the contracture, the surgeon makes a choice between a conservative program and complex surgical treatment.
Secondary contractures. The special pathogenesis of secondary contractures also determines a differentiated approach to choosing the optimal method of treatment for each patient.
With false secondary contractures, when movements in the PFS are limited due to extra-articular causes, the elimination of the latter makes it possible to restore movements in full.
With true unstable contractures, when there are already unexpressed secondary changes in the joint capsule, in addition to eliminating extra-articular causes of movement restriction, a sufficiently long course of conservative treatment is necessary. It usually includes the development of active and passive finger movements, thermal and other physiotherapy procedures.
However, with persistent true contractures, this is not enough. In most cases, the desired effect can be achieved only with the use of complex surgical treatment.
Basic principles and treatment regimens for primary desmogenic and secondary contractures of the metacarpophalangeal joints
Principle 1. Development of individual programs for each patient. These programs should be based on a comprehensive assessment of the initial clinical situation and the possibility of using modern methods treatment.Principle 2. Elimination of extra-articular (initial) causes of secondary contractures. Extra-articular causes of the development of PFS contractures most often have a tenogenic, dermatogenic or myogenic character. Often, all three causes are combined, and in general, the elimination of extra-articular causes of limitation of finger movements may require the surgeon to perform a wide variety of operations.
With tenogenic extensor contractures of the PJC, the extensor tendon is fixed to the surrounding tissues at a more proximal level. As a result of this, the volume of finger flexion decreases sharply (Fig. 27.10.2).

Rice. 27.10.2. The range of motion of the finger (a, b) when the extensor tendon is blocked at the level of the metacarpus.
F - accurate blocking of the extensor tendon; F is the possible displacement of the F point when pulling the flexor tendon (CO (explained in the text).
The cause of the contracture can be eliminated through various operations. The simplest intervention is tendolysis of the extensor tendon, which is indicated for a rather limited area of fibrosis surrounding the tendon tissues and in a satisfactory condition of the latter.
In more difficult situation tendolysis can be supplemented by isolating the tendon surface with a polymer film. With the consequences of severe injuries of the hand with widespread soft tissue fibrosis, as well as damage to the extensor tendons within the synovial canals, a satisfactory result of the operation can often be achieved only if the tendon (or tendon graft) freed from scars is surrounded by well-perfused tissues. Their transplantation (non-free or free) can be the most difficult element of the patient's surgical treatment.
The reason for the occurrence of tenogenic flexion contractures in the PFS is the fixation of the flexor tendons (or their damaged ends) to the walls of the bone-fibrous canals. In this case, the traction of the extensor tendons allows you to straighten the proximal phalanx only within certain limits (Fig. 27.10.3).

Rice. 27.10.3. The range of motion of the finger (a, b) when blocking the flexor tendons at the level of the metacarpus.
F - point of blocking of the flexor tendons; P is the possible displacement of point F during traction for the extensor tendon (CP) (explanation in the text).
Flexor tendon tendolysis or a one-stage tendoplasty may be performed to correct the cause of the blockage. It is important to emphasize that these two operations can give results only with a very limited lesion of the PFS capsule, when the amount of additional trauma to the PFS capsule associated with redressing is relatively small, and the pain syndrome in the postoperative period is not pronounced.
Otherwise, the need for relative rest of the affected hand precludes a full-fledged rehabilitation and inevitably leads to the loss of active function. That is why, in many cases, with a more extensive injury to the tendon flexor apparatus, the most correct are excision of the flexor tendons and implantation of polymer rods into the bone-fibrous canals of the fingers (the first stage of a two-stage tendoplasty). In this situation, the choice of the mode of postoperative development of movements is significantly expanded, and the achievement of the desired result becomes more guaranteed.
This approach often becomes uncontested in case of a combined injury of the flexor and extensor tendons.
The presence of extensive skin scars and tissue defects with severe fibrosis of the sliding structures involved in the affected area may require the surgeon to perform a wide variety of plastic surgeries: from Z-plasty of scars that limit the function to free transplantation of blood-supplying tissue complexes.
In some cases, the limitation of the movements of the fingers of the hand is associated with the loss of the ability of the muscles of the forearm to fully stretch due to a long stay in a non-functioning state. This problem may require both mobilization of the muscles involved in the scars and lengthening of the tendons.
Principle 3. Impact on the metacarpophalangeal joints to restore passive movements. After the extra-articular causes of limitation of mobility in the joint are eliminated, the surgeon is faced with the task of restoring passive movements in the joint by stretching (tearing, dissecting) the contracted parts of the articular capsule.
There are three main schemes for solving this problem:
1) redressing + immobilization with plaster splints;
2) capsulotomy + redressing + immobilization with plaster splints;
3) (capsulotomy +) redressing + use of an external fixation device (AVF).
Redressation + immobilization with plaster splints can be used in the simplest cases, when the main phalanges are relatively easily brought to the extreme positions and can be held in them without significant pressure on the surface of the finger.
The advantages of this approach include its simplicity and non-invasiveness, although the significant disadvantages of this treatment regimen limit its use. So, a gypsum splint gives only limited opportunities impact on the main phalanx of the finger due to the fact that the pressure of the plaster can cause local circulatory disorders in the tissues and severe pain. It is impossible to control the condition of the skin under the bandage, which does not allow diagnosing circulatory disorders in it in time. It is practically impossible to dosed gradual bending of the main phalanges of the finger, and the plaster splint itself requires frequent replacement.
In this regard, the use of this scheme of influence on the PFC is shown in the following cases:
- with relatively easily4 eliminated ("soft") contractures, when the skin over the joint turns white only with full flexion in the joint;
- with relatively short periods that have passed since the injury (2-3 months);
- in the absence of other significant damage to the hand.
Capsulotomy + redressing + immobilization with plaster splints. The expediency of including capsulotomy in the treatment regimen is most often determined on the operating table, if redressing does not allow transferring the proximal phalanx of the finger to the position of full flexion due to tissue resistance. This procedure is advisable only for less “hard” PFS contractures, when there is no pronounced traction after capsulotomy and redressing the main phalanx to its former position, provided that the skin over the joint turns white only in the last 30-degree sector of flexion of the main phalanx.
The last requirement is very important, as it determines the 4th principle of the treatment of contractures: the prevention of acute circulatory disorders in the skin and paraarticular tissues above the heads of the metacarpal bones that occur during forced flexion of the main phalanges of the finger. As mentioned above, with a long stay of the main phalanges in the extension position, not only the PPS capsule, but also the skin covering it lose elasticity.
With forced flexion of the main phalanges, the skin over the heads of the metacarpal bones is stretched and a white spot appears on it. Within this spot, a mechanical blockade of the microvasculature develops, the blood from which is squeezed out into the surrounding tissues. The boundaries of this zone are directly proportional to the degree of flexion in the MFC
(Fig. 27.10.4).

Rice. 27.10.4. Borders of the zone of blockade of the microvasculature of the tissues covering the head of the metacarpal bone (A, A"), arising from forced flexion of the proximal phalanx (b, c) during extensor contracture of the PPS (explanation in the text).
Prolonged retention of the finger in this position can lead to tissue necrosis, and the occurrence of this phenomenon excludes the fixation of the main phalanges in the position of full flexion. Yes, and this movement itself can only be gradual and involves constant monitoring of the state of blood supply to the skin.
The latter requirements can only be met when using the third scheme of influence on the PFC, which involves the use of AVF.
Capsulotomy + redress + use of AVF. Indications for the use of this treatment regimen are long-term "hard" contractures, when the skin over the PFS turns white already in the second (first) 30-degree flexion sector.
Operation technique. After elimination of extra-articular causes of contracture development, the surgeon performs dorsal-external capsulotomy and PFS redressing with proximal phalanges brought into full flexion position. Then, an external fixation device (AVF) is applied to the limb: two rings on the forearm and a half ring at the level of the metacarpus. In this case, the spokes are carried out so that the sliding structures of the forearm remain intact.
After fixing the hand in the middle physiological position, a special attachment is fixed to the distal ring, which makes it possible to provide dosed flexion of the main phalanges of the fingers by moving the spokes.
The latter are carried out at the level of the neck of the main phalanges closer to the dorsal cortical layer, bent accordingly and fixed in a special device (Fig. 27.10.5).

Rice. 27.10.5. The appearance of the hand, fixed in the AVF for gradual bending of the main phalanges.
Smooth bending of the main phalanges can be carried out until signs of skin malnutrition appear on the dorsum of the joint. In the following days, the main phalanges are smoothly brought into the position of full flexion, avoiding critical violations of the skin nutrition on the back of the hand (Fig. 27.10.6).

Rice. 27.10.6. Stages (a, b) of finger flexion in the metacarpophalangeal joints using an external fixation device (explanation in the text).
After a period of stabilization (from several hours to 1-3 days), the development of active (passive) movements in the PFS begins. To do this, the spokes going to the fingers are released from the clamps and, after a cycle of exercises, are again fixed in the flexion position. The frequency of such episodes and their duration are individual for each patient. After the movements in the MFC become sufficiently free in the extreme positions of the main phalanx of the finger, the AVF can be removed and replaced with plaster splints.
The use of AVF in the regimen for the treatment of persistent extensor contractures of the PFJ provides the surgeon with unique advantages. First of all, when the main phalanges are flexed, there is no pressure on the skin from the outside. Secondly, it becomes possible to gradually bring the main phalanges into the flexion position, as well as the implementation of a differentiated flexion program for each finger Thirdly, it provides constant control over the state of the skin over the joint.Finally, the intensity of the pain syndrome decreases due to the gradual movement of the fingers and the effect of the bending force not on the soft tissues, but on the bone.
These advantages make it possible to obtain good treatment results even with the most severe lesions of the hand.
Principle 5. Effective pain management. The main cause of pain in the treatment of extensor contractures of the PJC is stretching of the tissues of the articular capsule during flexion of the proximal phalanx. When an ischemic tissue area appears above the heads of the metacarpal bones, the pain increases sharply and can become unbearable. Finally, another component of the formation of pain syndrome is the development of postoperative inflammation caused by surgical trauma.
In the treatment of pain syndrome, it is important to distinguish two main directions. The first is the maximum reduction in the sources of pain impulses, which is achieved by preventing the formation of ischemic soft tissue foci with the help of anti-inflammatory therapy, as well as due to a strictly dosed rate of flexion of the main phalanges, adequate to the specific situation.
The second direction in treatment involves the use of analgesic drugs. With a significant scale of the operation, a good analgesic effect can be obtained with the help of blockades of the stellate ganglion.
Principle 6. Restoration of the function of the main kinematic chains of the finger. Restoration of passive movements in the PFS is usually only a fragment of the treatment, which involves the restoration of tendon function.
Only the restoration of the function of all the most important kinematic chains of the fingers of the hand allows the patient to acquire a full-fledged function.
IN AND. Arkhangelsky, V.F. Kirillov